
WHAT IS DEMENTIA?
Everything You Need to Know to Care for a Loved One with Dementia
Roughly 50 million people have dementia worldwide, and nearly 10 million new cases are diagnosed each year. It is one of the leading causes of disability and loss of independence in older adults.
Although clinical trials and ongoing research show some promising breakthroughs, there is no cure for dementia.
However, through knowledge and awareness of the disease, individuals diagnosed with dementia can get the specialized support and care they need to continue enjoying a high quality of life.

AN OVERVIEW OF DEMENTIA
Dementia is not a single disease. It is an umbrella term that includes a range of disorders caused by abnormal changes in the brain. Of those disorders, Alzheimer’s disease is the most prevalent. However, dementia can be a symptom of other diseases and medical conditions that affect the brain.
Although it typically affects older adults, dementia is not a normal part of aging. It can be either chronic or progressive, and is marked by changes in:
- Memory
- Comprehension
- Thinking
- Behavior
- Learning capacity
- Language
- Orientation
Decline in cognitive functioning can eventually affect the person’s independence and ability to perform everyday tasks like bathing, dressing and eating. As the disease progresses, it can have a profound physical, psychological, social, emotional and economic impact on the person and their loved ones.
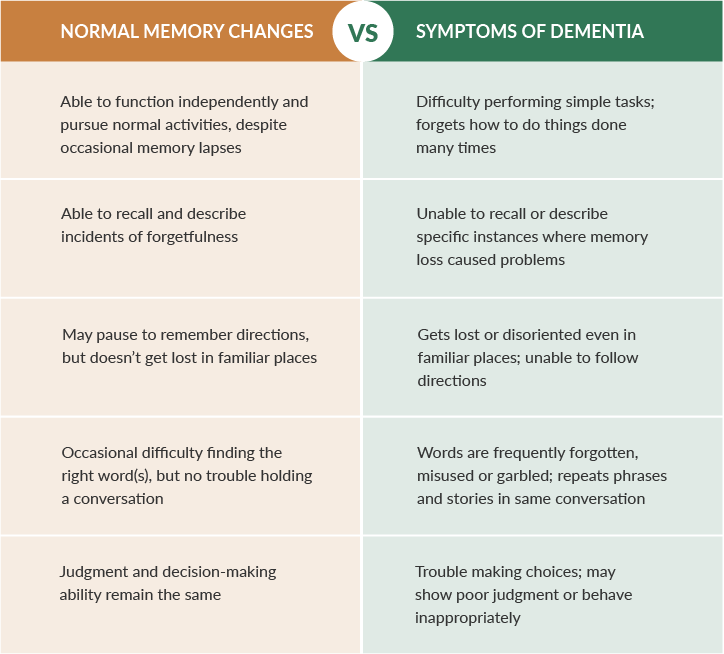
How does dementia differ from simple forgetfulness?
Occasional lapses in memory are a normal part of aging. For instance, forgetting where you left the keys or forgetting something on your grocery list. While they are frustrating, these types of memory lapses aren’t disabling. Conversely, the memory loss associated with dementia can be so persistent and severe that it impacts one’s work, relationships, social activities and daily life.
Dementia is often preceded by mild cognitive impairment (MCI). MCI involves problems with memory, language and thinking that go beyond forgetfulness and can signal a more serious issue.
Although MCI and normal memory loss appear similar, the distinction is in the degree of the symptoms. Below are some other key differences between age-related memory loss and dementia.
Signs and symptoms
Symptoms of dementia can vary greatly depending on the cause and type of dementia. They often appear in clusters and progress over time.
However, even among different dementia types, common cognitive and psychological changes exist.
COGNITIVE CHANGES
- Memory loss, usually noticed by someone else
- Difficulty communicating or finding words
- Difficulty with visual and spatial abilities, such as getting lost while driving
- Difficulty reasoning or problem-solving
- Difficulty handling complex tasks
- Difficulty with planning and organizing
- Difficulty with coordination and motor functions
- Confusion and disorientation
PSYCHOLOGICAL CHANGES
- Personality changes
- Depression
- Anxiety
- Inappropriate behavior
- Paranoia
- Agitation
- Hallucinations

Risk factors for dementia
Researchers have identified dementia risk factors that are associated with particular behaviors. This is good news for those who are concerned about the possibility of developing dementia; if you change certain behaviors and control certain conditions, you can reduce your risk.


GETTING A DIAGNOSIS
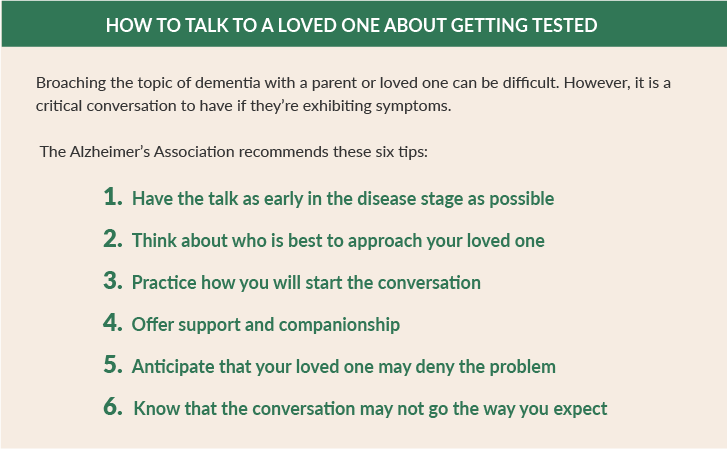
 Early diagnosis is key to treating dementia and ultimately maintaining a good quality of life. When memory lapses become frequent or noticeable enough to cause concern, it’s time to see a doctor.
Early diagnosis is key to treating dementia and ultimately maintaining a good quality of life. When memory lapses become frequent or noticeable enough to cause concern, it’s time to see a doctor.
If you’re worried about a loved one’s memory, but aren’t sure whether it warrants deeper concern, a simple home test can detect early signs of cognitive impairment. However, even if the results suggest impairment, they are not a diagnosis.
They can, however, help a doctor understand how well your brain is working.
There is no one test for diagnosing dementia. Through a thorough medical history, physical examination and lab tests, a physician can assess risk factors, evaluate symptoms and eliminate other possible causes.

TYPES OF DEMENTIA
Doctors can determine whether a person has dementia with a high level of certainty. However, due to overlap in symptoms, it can be more challenging to determine the specific type of dementia. That may require the expertise of a neurologist, geropsychologist or another specialist.
There are many different types of dementia, but some are more common than others
Alzheimer’s
The most common type of dementia, Alzheimer’s disease accounts for 60% to 80% of all dementia cases.
Although the majority of people with Alzheimer’s are older, approximately 200,000 Americans under the age of 65 have early-onset Alzheimer’s disease.
While the exact cause of Alzheimer’s isn’t fully understood, scientists believe it’s likely a combination of factors, including genetics, lifestyle and environment.
Microscopic changes in the brain begin long before the first signs of memory loss. It’s believed that two abnormal structures play a critical role in Alzheimer’s disease:
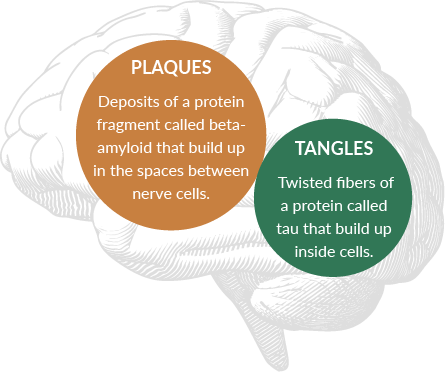
Although most people develop some plaques and tangles as they age, those with Alzheimer’s develop far more. Scientists haven’t pinpointed the role plaques and tangles play in Alzheimer’s, but believe they may block communication among neurons, disrupting critical processes.
Because it typically begins in the part of the brain that affects learning, a common early symptom is difficulty recalling newly learned information (aka short-term memory loss). As it progresses, other symptoms may include:
- Memory loss
- Disorientation
- Difficulty completing familiar tasks
- Confusion with time or place
- Problems with words in speaking or writing
- Changes in mood and personality
Vascular Dementia
Vascular dementia is a decline in cognitive skills caused by blocked or reduced blood flow to various parts of the brain. Accounting for 5% to 10% of dementia cases, it is considered the second most common cause of dementia.
Vascular dementia can develop suddenly after a stroke, which blocks major blood vessels in the brain. Other times it begins as mild changes that gradually worsen as a result of multiple minor strokes or another condition that affects smaller blood vessels and nerve fibers in the brain.
Symptoms can vary depending on the severity of damage to the blood vessels and the parts of the brain it affects. Common symptoms include:
- Confusion
- Trouble paying attention and concentrating
- Reduced ability to organize thoughts or actions
- Decline in ability to analyze a situation, develop an effective plan and communicate it to others
- Difficulty deciding what to do next
- Memory trouble
- Restlessness and agitation
- Unsteady gait
- Sudden or frequent urge to urinate or inability to control passing urine
- Depression or apathy
These symptoms may be most apparent when they come on suddenly after a stroke.
Lewy Body Dementia
Lewy Body Dementia is a progressive dementia that leads to a decline in thinking, reasoning and independent function. It is caused by abnormal microscopic protein deposits in the brain that damage cells over time.
It is named after German neurologist Friedrich H. Lewy, who discovered these microscopic protein deposits (aka Lewy bodies) in 1912.
Common symptoms of Lewy Body Dementia include:
- Changes in thinking and reasoning
- Hunched posture, balance problems and rigid muscles
- Visual hallucinations and/or delusions
- Trouble interpreting visual information
- Confusion that may vary in severity from one day to the next
- Memory loss but not as severe as in Alzheimer’s disease
Frontotemporal Dementia
Frontotemporal dementia (FTD) is a term that describes a group of brain disorders that affect the frontal and temporal lobes. Atrophy of these areas results in progressive nerve cell damage that impacts behavior, personality and language.
Frontotemporal dementia can be categorized by subtypes:
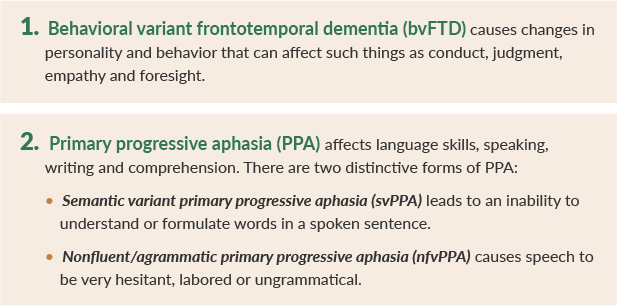
FTD has been linked to genetic mutations, with roughly a third of all cases being inherited. Other than family history, there are no known risk factors.
Often misdiagnosed as a psychiatric problem or Alzheimer’s disease, FTD is the most common cause of dementia in people under age 60. Symptoms often appear in clusters and get progressively worse over time. Common symptoms include:
- Poor judgment
- Loss of empathy
- Socially inappropriate behavior
- Lack of inhibition
- Repetitive compulsive behavior
- Inability to concentrate or plan
- Frequent, abrupt mood changes
- Speech difficulties
- Problems with balance or movement
- Memory loss
Previously called Pick’s disease (a name still used) after Arnold Pick, the physician who first described the disorder in 1892, frontotemporal dementia is sometimes referred to as frontotemporal disorders, frontotemporal degenerations and frontal lobe disorders.
Other Types of Dementia
In addition to those covered above, many other types of dementia exist:
Parkinson’s disease
Advanced Parkinson’s disease often develops into dementia. Early signs include problems with reasoning and judgment, as well as irritability. Additionally, as the disease progresses, many people become depressed or paranoid, while others have trouble with language.
Creutzfeldt-Jakob disease (CJD)
This is one of the rarest forms of dementia – only one in one million people are diagnosed with it annually. CJD progresses very quickly. Symptoms are similar to other forms of dementia and include agitation, depression, confusion and memory loss. It also affects the body, causing twitching and muscle stiffness.
Wernicke-Korsakoff syndrome
Wernicke’s disease and Korsakoff syndrome are distinct disorders that are usually grouped as one condition. Though technically not a form of dementia, because of the similarity in symptoms it’s often classified with dementia. Alcoholism or chronic alcohol misuse is the most common cause. It can also be linked to diet deficiencies or other medical conditions that interfere with the absorption of vitamin B-1.
Mixed dementia
Mixed dementia is when an individual has more than one type of dementia. Although it’s very common, up to 45% of people with dementia have mixed dementia but don’t know it. The most common combination is vascular dementia and Alzheimer’s.
Normal pressure hydrocephalus (NPH)
A condition that causes a buildup of excess fluid and pressure in the brain, NPH can lead to damage that results in dementia symptoms. Causes range from injury and infection to bleeding and brain tumors. NPH is one type of dementia that can sometimes be cured with surgery.
Huntington’s disease
A genetic condition that causes a premature breakdown of the brain’s nerve cells, Huntington’s disease leads to dementia. There are two types: juvenile and adult onset. The juvenile form causes symptoms in childhood or adolescence. The adult form typically presents in the individual’s 30s or 40s.
Symptoms of Huntington’s disease dementia mirror those of other forms of dementia and include apathy, irritability, severe depression and memory problems.

Stages of Dementia
Once an individual is diagnosed with dementia, and the specific type has been identified, a physician can measure how advanced it is.
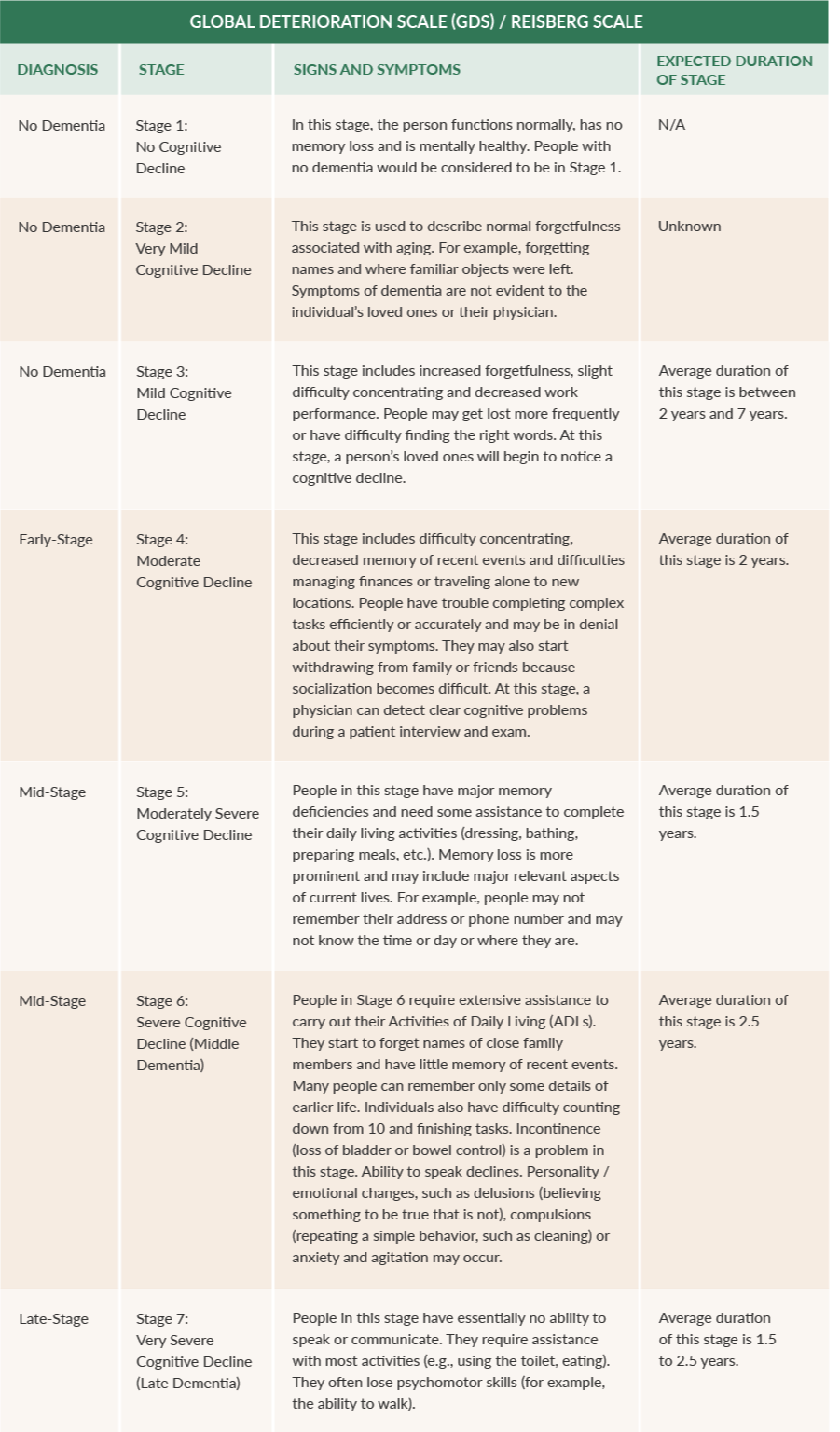
The most commonly used scale is the GDS, or the Global Deterioration Scale for Assessment of Primary Degenerative Dementia.
The GDS scale divides the disease into seven stages based on the person’s cognitive decline. In stages 1-3, people do not typically exhibit enough symptoms for a diagnosis. By the time a diagnosis is made, a dementia patient is typically in stage 4 or beyond.

COMMON DEMENTIA-RELATED BEHAVIORS
Caring for a loved one with dementia can be overwhelming, but it can be even more challenging if they develop unusual and upsetting behaviors.
Recognizing that behavioral changes are a common part of the disease can help in dealing with them as they occur.
Some common behaviors associated with dementia include:
- Aggression
- Anger
- Apathy or disinterest
- Communication problems
- Mood swings
- Night-time waking
- Pacing
- Physical acting out (hitting)
- Restlessness
- Verbal abuse

THESE BEHAVIORS CAN BE GROUPED INTO THREE AREAS:
Personality Changes
For those living with dementia and their caregivers, one of the more difficult aspects of the disease can be changes in personality. From anger and irritability to mood swings, they may behave quite differently from the person their loved ones have come to know.
In the early stages of dementia, the person is often aware of these changes. Understandably, that can trigger feelings of anxiety, fear and depression. As it progresses, the changes may become more pronounced and appear with more frequency.
It’s important for loved ones to realize that it’s not personal, and that it’s the disease causing this behavior. Approaching the situation with empathy and a better understanding of what’s behind these changes can help make coping with them easier.
Sundowning
It’s common for individuals with dementia to show a marked increase in confusion and agitation in the late afternoon or early evening hours. This is known as Sundown Syndrome, or sundowning.
In severe cases, sundowning may include extreme anger and agitation along with anxiety, aggression and depression. These symptoms typically fade overnight and during the daytime hours until the cycle begins again at sundown.
Though experts aren’t sure what causes Sundown Syndrome, it may be tied to disruptions in the body’s circadian rhythms brought on by an internal shift that causes brain activity levels to “shut down” earlier in the evening.
While there is no cure for Sundown Syndrome, you can take steps to minimize the symptoms.
Wandering
Wandering is one of the most common symptoms of dementia. Because it can result in the person getting lost, it’s also one of the most concerning symptoms.
Wandering can happen at any stage of dementia, and for a variety of reasons, including:
- Reacting to stress or fear
- Searching for someone or something
- Boredom that leads them to look for something to do
- Attending to basic needs, such as for a bathroom or food
- Following past routines, such as going to work or shopping
Although it can potentially present safety issues, wandering is not necessarily harmful if it happens in a safe and controlled environment.

CARING FOR SOMEONE WITH DEMENTIA AT HOME
 More than 16 million people in the United States care for someone with dementia. It’s a true act of caring and compassion that can make a huge difference in a loved one’s quality of life.
More than 16 million people in the United States care for someone with dementia. It’s a true act of caring and compassion that can make a huge difference in a loved one’s quality of life.
Caring for a loved one with dementia at home can be difficult depending on the severity of their cognitive and behavioral symptoms. However, you can help ensure the person’s safety and improve their daily life.
Keeping them safe
People with Alzheimer’s disease or other forms of dementia literally see the world in a new, often confusing way. Making a home safe and easier to navigate is key to their well-being. To keep loved one’s safe, caregivers can:
- Install alarms and locks to prevent them from wandering off
- Remove locks to doors, such as the bathroom, to prevent your loved one from getting locked in or locking you out
- Install grab bars and non-skid bath mats
- Secure or lock away medicines
- Use a GPS device to help locate the person quickly
Keeping them oriented with visual cues
Individuals with dementia may experience mild to severe disorientation, confusion and wandering. Using visual cues can help with wayfinding and provide prompts to help them perform daily tasks.
Below are examples of helpful visual cues:
- Use pictures and/or labels to help them identify and recognize items.
- Use high-contrast colors to make things stand out.
- Use signs to give directions, such as “bathroom down the hall,” or use arrows and pictures to illustrate it.
- Link colors to rooms. For instance, make signs or labels for the bathroom blue (water) and those related to the outdoors green (grass).
- Place essential items where they’ll find them. For example, put their toothbrush and toothpaste on the vanity, leave lunch on the table or lay out their clothes on the bed.
Keeping them engaged
Keeping a person with dementia active and engaged is key to maintaining quality of life. Encouraging them to continue to pursue hobbies and interests can help reduce anxiety, provide a sense of accomplishment, stir memories and foster emotional connections.
The goal should be to provide meaningful activities, not simply fill time. Focus on the activity rather than the results – what matters most is that your loved one is actively engaged.


WHEN IT’S TIME TO FIND ANOTHER SOLUTION
While caring for a loved one with dementia can be rewarding, as the disease advances it may become more challenging, or even all-consuming.
While many caregivers want to continue caring for their loved ones at home for as long as possible, there may come a time when it’s in everyone’s best interest to consider other options.
The decision to move a loved one into residential care is never easy and may bring on feelings of guilt. However, the best way to support their health and safety is to ensure they’re in a place that can provide the best possible care.
Here are six signs that it’s the right time for a specialized care facility:
- 1. Increased aggression
- 2. Caregiver stress that’s unmanageable or impacts your health
- 3. Escalating care needs that are beyond your abilities
- 4. Concerns about home safety
- 5. Sundowning that severely disrupts family routines
- 6. Frequent wandering
What to look for in a facility
Choosing a care facility requires time, research and consideration. Here are four things Dementia Care Central recommends considering:

Before making a decision, it’s always best to ask for recommendations from trusted friends and colleagues, review state inspection reports, talk with current residents and/or their family members and take a tour.
Memory care center vs. long-term care facility
 When considering residential care for a loved one with dementia, it’s important to understand the difference between a typical memory care facility and a specialized memory care center.
When considering residential care for a loved one with dementia, it’s important to understand the difference between a typical memory care facility and a specialized memory care center.
There are a number of different types of long-term care options, including assisted living, skilled nursing facilities and memory care centers. Each offers varying degrees of independence, expertise, medical attention and supervision.
While some assisted living and skilled nursing facilities might be sufficient for individuals in the early stages of dementia, they’re not always ideal for those in advanced stages.
A specialized memory care center, on the other hand, offers expertise for individuals with dementia. It provides clinical care and supervision from staff trained to meet the unique needs of those living with dementia.
In addition to a higher level of care, a specialized memory care center also provides a variety of activities designed to keep residents engaged and stimulate memory.
Visit Our Specialized Memory Care Center
Join Us for a Virtual or In-Person Tour
